A 65 year old male with SOB
1 st August,2022.
A 65 year old male patient from Gundrampally village, Chityala district who used to be a toddy climber by occupation came to the casuality with
C/o Shortness of breath since 3 days
Associated symptoms are
Weakness in left upper limb and lower limb since 8 days
Difficulty in walking since 8 days
Involuntary defecation and micturition since 5 days
History of presenting illness
As explained by the patients' younger son
Patient was apparently asymptomatic 10 years back then one day early in the morning while waking up he noticed weakness in the left upper limb and lower limb and couldn't support himself properly.
2 days later he started using Ayurvedic medicine for the weakness, which progressively improved and he got completely alright within a month and got back to his daily routine
Patient had a normal life style until 8 days back.
8 days back at 12 am patient woke up to micturate and noticed that he is having a similar weakness in the left upper and lower limb like previous and couldn't support himself.
5 days back he started passing loose stools and micturating involuntarily but he had knowledge of passing them yet couldn't hold them
Patient conscious during all these events
They visited a local RMP doctor for weakness and difficulty in walking for which the RMP doctor infused IV potassium.
The following night patient woke up with grade 4 shortness of breath associated with palpitations at around 12 am for which he was brought to the hospital.
Patient was conscious at the time of admission but gradually felt drowsy and now the patient can listen to us and respond through actions but can not speak.
Past history
K/c/o Hypertension since 10 years and was on regular medication( T. Atenolol 50 mg po OD) until 2months back when he started taking meds irregularly
Not a k/c/o Diabetes mellitus, Tuberculosis, Asthma, Epilepsy, CAD.
Personal history
Patient had a good appetite with a mixed diet involving mostly rice and non vegetarian food.
He sleeps for 7 hours from around 10pm to 5 am but wakes up to smoke beedi multiple times during night.
Bowel and bladder movements irregular
Has a habit of smoking since many years and smokes nearly 30 beedis in a day daily
Occasional alcoholic.
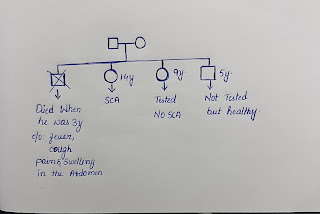
Family history- No other family members have similar complaints.
Treatment history - Tab. Atenolol 50 mg OD for the past 10 years.
General physical examination
Patient is drowsy
No pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy, edema.
Vitals
Temperature - Afebrile currently but had a fever spike during night.
Pulse - 110 bpm
Respiratory rate - 20cpm
Blood pressure - 120/70 mmHg
SpO2 - 97%
GRBS - 218 mg/dL
Systemic examination
Respiratory system - Shortness of breath grade 4, BAE present with Inspiratory crepitus and expiratory ronchi
CVS - S1, S2 heard.
Abdomen - Soft, Non tender
CNS - patient is drowsy and arousable
GCS - E2V2M4
Power Rt Lt
Upper limb 4/5 0/5
Lower limb 4/5 0/5
Tone Rt Lt
Upper limb Normal Decreased
Lower limb Normal Decreased
Reflexes Right Left
Biceps ++ ++
Triceps ++ ++
Wrist + +
Knee ++ ++
Ankle + +
Plantar withdrawal extensor


Comments
Post a Comment