15 year old boy suffering with CKD and SOB
PRESENTING COMPLAINTS:
A 15 yr old boy, resident of Nalgonda, studying 9 th class came to the casualty 6 days ago with c/o SOB
History of presenting illness:
Patient was apparently asymptomatic 2 months back then he developed fever which was sudden in onset,intermittent associated with chills and subsided on taking medication, which was followed by vomiting (2-3 episodes every day) which occurs after having dinner, it is associated with food particles and not associated with blood He had these episodes for 10 to 15 days.
They went to the local hospital in nalgonda and the patient was found to have 62 mg/dl urea level and creatinine level was 8.3mg/dl , so they referred him to Hyderabad hospital, where they had been told that he has CKD, in a day urea level had raised to 135mg/dl and creatinine level had increased to 10.7.
They have immediately started him on dialysis. 5 sessions of HD were done and he felt better.
5 days ago he came to the hospital with c/O of shortness of breath and chest pain which was dragging type occurs only during episode of SOB.
No C/O palpitations, syncope attack
No C/O decreased urine
No C/O decreased urine output , pedal edema, facial Puffiness.
After getting admitted to the hospital he underwent 3 sessions of hemodialysis on 12 th, 13 th and 14 th of November during which his creatinine and urea levels decreased, but his urea levels increased again on 15 th.
After dialysis patient felt better.
Past history:
Hypertensive since 1 month and is on Tab.AMLONG 5 mg
History of 3 transfusions 1 month back
Not a K/C/O DM ,Asthma ,epilepsy ,thyroid disorders
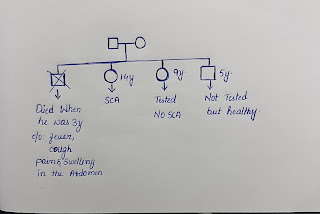
Family History :
No H/O renal problems in their whole family.
His paternal grandfather is diabetic and hypertensive
Personal History:
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel movements : regular
Bladder movements : regular
No history of alcohol consumption or smoking history
General Examination:
Patient is conscious, coherent , cooperative
Pallor -present
Icterus -absent
Clubbing-absent
Cyanosis -absent
Generalised Lymphadenopathy-absent
Pedal Edema -absent
O/E:
Vitals:
On day 1
Temperature : 98.6°F
BP: 140/90 mm Hg in right upper arm in supine position
PR: 76 bpm
RR: 20 cycles per minute
Spo2: 88% on room air
96% at 4 litres of O2
Vitals:
Temperature : afebrile
Pulse rate : 96 bpm
Respiratory rate : 24 cycles /min
BP : 140/100 mm of Hg
SpO2 : 86 % at Room air .
GRBS : 121 mg%
Systemic Examination:
CVS: S1,S2 heard no murmurs
CNS: normal
RS :
Bilateral Air Entry - present
Bilateral crepitations heard at IAA and ISA.
No wheeze .
PA:
Soft ,non tender
Bowel sounds +
CNS:
NAD
Investigations :
On day 1
HEMOGRAM :
Hb - 8.7
TLC - 7800
N - 50
L - 40
M - 05
E - 05
B -00
Pcv - 25.1
RBC - 3.19
Plt - 1.2
MCV -78.7
MCH -27.3
MCHC - 34.7
Blood group : A positive
CUE :
Pale yellow
Albumin - 3+
Sugar -Trace
Pus cells- 6 to 8
Epithelial cells -3to 4
FBS - 78
RFT:
Creatinine - 9.2
Urea - 119
UA - 5.5
Na - 141
K - 5.6
Cl - 101
LFT :
TB - 0.79
Db - 0.19
AST - 17
ALT - 10
ALP - 201
TP - 5.8
ALB - 3.4
A/G - 1.36
15-11-2021
Hb-6. 3 gm/dl
Platelet count -1. 7 lakh/cu.mm
Lymphocytes-17%
Neutrophiles-78%
urea-107
Creatinine-1. 6
Uric acids-2. 1
Calcium-7. 5
Phosphorus-8. 0
Sodium-148
Potassium-2. 9.
USG finding :
Bilateral grade 1 rpd changes
Treatment:
T. NICARDIA - 10 mg , TID
T. LASIX- 40mg TID
T. Metal 50mg OD
T. CILINEDEFIONE 10mg OD
T. TELMA 20mg BD
T. LIVOGIN BD
Syp- GRILLNKTUS 15ml TID
NEB- BUDECORT 12th hourly
NEB-IPRAVENT 8th hourly
Fluid restriction
Salt restriction
MANITOR UTULS 2nd hourly


Comments
Post a Comment